| Citation: | Kuang RF, Wang Z, Ma L et al. Smart photonic wristband for pulse wave monitoring. Opto-Electron Sci 3, 240009 (2024). doi: 10.29026/oes.2024.240009 |
-
Abstract
Real-time acquisition of human pulse signals in daily life is clinically important for cardiovascular disease monitoring and diagnosis. Here, we propose a smart photonic wristband for pulse signal monitoring based on speckle pattern analysis with a polymer optical fiber (POF) integrated into a sports wristband. Several different speckle pattern processing algorithms and POFs with different core diameters were evaluated. The results indicated that the smart photonic wristband had a high signal-to-noise ratio and low latency, with the measurement error controlled at approximately 3.7%. This optimized pulse signal could be used for further medical diagnosis and was capable of objectively monitoring subtle pulse signal changes, such as the pulse waveform at different positions of Cunkou and pulse waveforms before and after exercise. With the assistance of artificial intelligence (AI), functions such as gesture recognition have been realized through the established prediction model by processing pulse signals, in which the recognition accuracy reaches 95%. Our AI-assisted smart photonic wristband has potential applications for clinical treatment of cardiovascular diseases and home monitoring, paving the way for medical Internet of Things-enabled smart systems.-
Keywords:
- smart healthcare /
- specklegram /
- pulse monitoring /
- gesture recognition /
- artificial intelligence /
- wearable sensor
-

-
References
[1] Chen SW, Qi JM, Fan SC et al. Flexible wearable sensors for cardiovascular health monitoring. Adv Healthc Mater 10, 2100116 (2021). doi: 10.1002/adhm.202100116 [2] Vogel B, Acevedo M, Appelman Y et al. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet 397, 2385–2438 (2021). doi: 10.1016/S0140-6736(21)00684-X [3] Gilgen-Ammann R, Schweizer T, Wyss T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur J Appl Physiol 119, 1525–1532 (2019). doi: 10.1007/s00421-019-04142-5 [4] Zheng Q, Tang QZ, Wang ZL et al. Self-powered cardiovascular electronic devices and systems. Nat Rev Cardiol 18, 7–21 (2021). doi: 10.1038/s41569-020-0426-4 [5] Tan PC, Xi Y, Chao SY et al. An artificial intelligence-enhanced blood pressure monitor wristband based on piezoelectric nanogenerator. Biosensors 12, 234 (2022). doi: 10.3390/bios12040234 [6] Chen SW, Wu N, Lin SZ et al. Hierarchical elastomer tuned self-powered pressure sensor for wearable multifunctional cardiovascular electronics. Nano Energy 70, 104460 (2020). doi: 10.1016/j.nanoen.2020.104460 [7] Meng KY, Xiao X, Wei WX et al. Wearable pressure sensors for pulse wave monitoring. Adv Mater 34, 2109357 (2022). doi: 10.1002/adma.202109357 [8] Chu Y, Zhong JW, Liu HL et al. Human pulse diagnosis for medical assessments using a wearable piezoelectret sensing system. Adv Funct Mater 28, 1803413 (2018). doi: 10.1002/adfm.201803413 [9] Sun YZ, Zhang ZQ, Zhou Y et al. Wearable strain sensor based on double-layer graphene fabrics for real-time, continuous acquirement of human pulse signal in daily activities. Adv Mater Technol 6, 2001071 (2021). doi: 10.1002/admt.202001071 [10] Ouyang H, Tian JJ, Sun GL et al. Self-powered pulse sensor for antidiastole of cardiovascular disease. Adv Mater 29, 1703456 (2017). doi: 10.1002/adma.201703456 [11] Wang SP, Wang XY, Wang S et al. Optical-nanofiber-enabled gesture-recognition wristband for human-machine interaction with the assistance of machine learning. Adv Intell Syst 5, 2200412 (2023). doi: 10.1002/aisy.202200412 [12] Chen GR, Au C, Chen J. Textile triboelectric nanogenerators for wearable pulse wave monitoring. Trends Biotechnol 39, 1078–1092 (2021). doi: 10.1016/j.tibtech.2020.12.011 [13] Roy K, Ghosh SK, Sultana A et al. A self-powered wearable pressure sensor and pyroelectric breathing sensor based on GO interfaced PVDF nanofibers. ACS Appl Nano Mater 2, 2013–2025 (2019). [14] Yan C, Deng WL, Jin L et al. Epidermis-inspired ultrathin 3D cellular sensor array for self-powered biomedical monitoring. ACS Appl Mater Interfaces 10, 41070–41075 (2018). doi: 10.1021/acsami.8b14514 [15] Zhu HH, Liu A, Luque HL et al. Perovskite and conjugated polymer wrapped semiconducting carbon nanotube hybrid films for high-performance transistors and phototransistors. ACS Nano 13, 3971–3981 (2019). doi: 10.1021/acsnano.8b07567 [16] Ma C, Xu D, Huang YC et al. Robust flexible pressure sensors made from conductive micropyramids for manipulation tasks. ACS Nano 14, 12866–12876 (2020). doi: 10.1021/acsnano.0c03659 [17] Wang S, Chen GR, Niu SY et al. Magnetic-assisted transparent and flexible percolative composite for highly sensitive piezoresistive sensor via hot embossing technology. ACS Appl Mater Interfaces 11, 48331–48340 (2019). doi: 10.1021/acsami.9b16215 [18] Yang TT, Jiang X, Zhong YJ et al. A wearable and highly sensitive graphene strain sensor for precise home-based pulse wave monitoring. ACS Sens 2, 967–974 (2017). doi: 10.1021/acssensors.7b00230 [19] Xiong YX, Shen YK, Tian L et al. A flexible, ultra-highly sensitive and stable capacitive pressure sensor with convex microarrays for motion and health monitoring. Nano Energy 70, 104436 (2020). doi: 10.1016/j.nanoen.2019.104436 [20] Guan FY, Xie Y, Wu HX et al. Silver nanowire-bacterial cellulose composite fiber-based sensor for highly sensitive detection of pressure and proximity. ACS Nano 14, 15428–15439 (2020). doi: 10.1021/acsnano.0c06063 [21] Lin QP, Huang J, Yang JL et al. Highly sensitive flexible iontronic pressure sensor for fingertip pulse monitoring. Adv Healthc Mater 9, 2001023 (2020). doi: 10.1002/adhm.202001023 [22] Min R, Liu ZY, Pereira L et al. Optical fiber sensing for marine environment and marine structural health monitoring: a review. Opt Laser Technol 140, 107082 (2021). doi: 10.1016/j.optlastec.2021.107082 [23] Wang X, Zhou HY, Chen MH et al. Highly sensitive strain sensor based on microfiber coupler for wearable photonics healthcare. Adv Intell Syst 5, 2200344 (2023). doi: 10.1002/aisy.202200344 [24] Jia DG, Chao J, Li S et al. A fiber bragg grating sensor for radial artery pulse waveform measurement. IEEE Trans Biomed Eng 65, 839–846 (2018). doi: 10.1109/TBME.2017.2722008 [25] Pant S, Umesh S, Asokan S. A novel approach to acquire the arterial pulse by finger plethysmography using fiber bragg grating sensor. IEEE Sens J 20, 5921–5928 (2020). doi: 10.1109/JSEN.2020.2973342 [26] Li HQ, An ZX, Zhang S et al. Fully photonic integrated wearable optical interrogator. ACS Photonics 8, 3607–3618 (2021). doi: 10.1021/acsphotonics.1c01236 [27] Li LY, Li YP, Yang LY et al. Continuous and accurate blood pressure monitoring based on wearable optical fiber wristband. IEEE Sens J 21, 3049–3057 (2021). doi: 10.1109/JSEN.2020.3027919 [28] Smith DL, Nguyen LV, Ottaway DJ et al. Machine learning for sensing with a multimode exposed core fiber specklegram sensor. Opt Express 30, 10443–10455 (2022). doi: 10.1364/OE.443932 [29] Murray MJ, Davis A, Kirkendall C et al. Speckle-based strain sensing in multimode fiber. Opt Express 27, 28494–28506 (2019). doi: 10.1364/OE.27.028494 [30] Gu LL, Gao H, Hu HF. Demonstration of a learning-empowered fiber specklegram sensor based on focused ion beam milling for refractive index sensing. Nanomaterials 13, 768 (2023). doi: 10.3390/nano13040768 [31] Chen W, Feng F, Chen DH et al. Precision non-contact displacement sensor based on the near-field characteristics of fiber specklegrams. Sens Actuators A Phys 296, 1–6 (2019). doi: 10.1016/j.sna.2019.06.010 [32] Qureshi MM, Liu Y, Mac KD et al. Quantitative blood flow estimation in vivo by optical speckle image velocimetry. Optica 8, 1092–1101 (2021). doi: 10.1364/OPTICA.422871 [33] Bennett A, Beiderman Y, Agdarov S et al. Monitoring of vital bio-signs by analysis of speckle patterns in a fabric-integrated multimode optical fiber sensor. Opt Express 28, 20830–20844 (2020). doi: 10.1364/OE.384423 [34] Min R, Hu XH, Pereira L et al. Polymer optical fiber for monitoring human physiological and body function: a comprehensive review on mechanisms, materials, and applications. Opt Laser Technol 147, 107626 (2022). doi: 10.1016/j.optlastec.2021.107626 [35] Shi Y, Tangdiongga E, Koonen AMJ et al. Plastic-optical-fiber-based in-home optical networks. IEEE Commun Mag 52, 186–193 (2014). [36] Talataisong W, Gorecki J, van Putten LD et al. Hollow-core antiresonant terahertz fiber-based TOPAS extruded from a 3D printer using a metal 3D printed nozzle. Photonics Res 9, 1513–1521 (2021). doi: 10.1364/PRJ.420672 [37] Woyessa G, Fasano A, Markos C et al. Zeonex microstructured polymer optical fiber: fabrication friendly fibers for high temperature and humidity insensitive Bragg grating sensing. Opt Mater Express 7, 286–295 (2017). doi: 10.1364/OME.7.000286 [38] Theodosiou A, Min R, Leal-Junior AG et al. Long period grating in a multimode cyclic transparent optical polymer fiber inscribed using a femtosecond laser. Opt Lett 44, 5346–5349 (2019). doi: 10.1364/OL.44.005346 [39] Liu L, Zheng J, Deng SJ et al. Parallel polished plastic optical fiber-based SPR sensor for simultaneous measurement of RI and temperature. IEEE Trans Instrum Meas 70, 9508308 (2021). [40] Leal-Junior AG, Frizera A, Marques C et al. Optical fiber specklegram sensors for mechanical measurements: a review. IEEE Sens J 20, 569–576 (2020). doi: 10.1109/JSEN.2019.2944906 [41] Avellar L, Delgado G, Marques C et al. Polymer optical fiber-based smart garment for impact identification and balance assessment. IEEE Sens J 21, 20078–20085 (2021). doi: 10.1109/JSEN.2021.3098475 [42] Cooley JW, Lewis PAW, Welch PD. The fast Fourier transform and its applications. IEEE Trans Ed 12, 27–34 (1969). doi: 10.1109/TE.1969.4320436 [43] Jokinen H, Ollila J, Aumala O. On windowing effects in estimating averaged periodograms of noisy signals. Measurement 28, 197–207 (2000). doi: 10.1016/S0263-2241(00)00013-0 [44] Di Stefano L, Mattoccia S, Tombari F. ZNCC-based template matching using bounded partial correlation. Pattern Recognit Lett 26, 2129–2134 (2005). doi: 10.1016/j.patrec.2005.03.022 [45] Kumar CK, Manaswini M, Maruthy KN et al. Association of Heart rate variability measured by RR interval from ECG and pulse to pulse interval from photoplethysmography. Clin Epidemiol Global Health 10, 100698 (2021). doi: 10.1016/j.cegh.2021.100698 [46] Quer G, Gouda P, Galarnyk M et al. Inter- and intraindividual variability in daily resting heart rate and its associations with age, sex, sleep, BMI, and time of year: retrospective, longitudinal cohort study of 92, 457 adults. PLoS One 15, e0227709 (2020). doi: 10.1371/journal.pone.0227709 [47] Neha, Sardana HK, Kanwade R, Tewary S. Arrhythmia detection and classification using ECG and PPG techniques: a review. Phys Eng Sci Med 44, 1027–1048 (2021). doi: 10.1007/s13246-021-01072-5 [48] Rodríguez-Cuevas A, Peña ER, Rodríguez-Cobo L et al. Low-cost fiber specklegram sensor for noncontact continuous patient monitoring. J Biomed Opt 22, 037001 (2017). doi: 10.1117/1.JBO.22.3.037001 [49] Hill KO, Tremblay Y, Kawasaki BS. Modal noise in multimode fiber links: theory and experiment. Opt Lett 5, 270–272 (1980). doi: 10.1364/OL.5.000270 [50] Wang J, Zhu YR, Wu ZY et al. Wearable multichannel pulse condition monitoring system based on flexible pressure sensor arrays. Microsyst Nanoeng 8, 16 (2022). doi: 10.1038/s41378-022-00349-3 [51] Tyan CC, Liang WM, Shy HY et al. How to standardize 3 finger positions of examiner for palpating radial pulses at wrist in traditional Chinese medicine. Acupunct Electrother Res 32, 87–96 (2007). -
Supplementary Information
Supplementary information for Smart photonic wristband for pulse wave monitoring 
-
Access History

Article Metrics
-
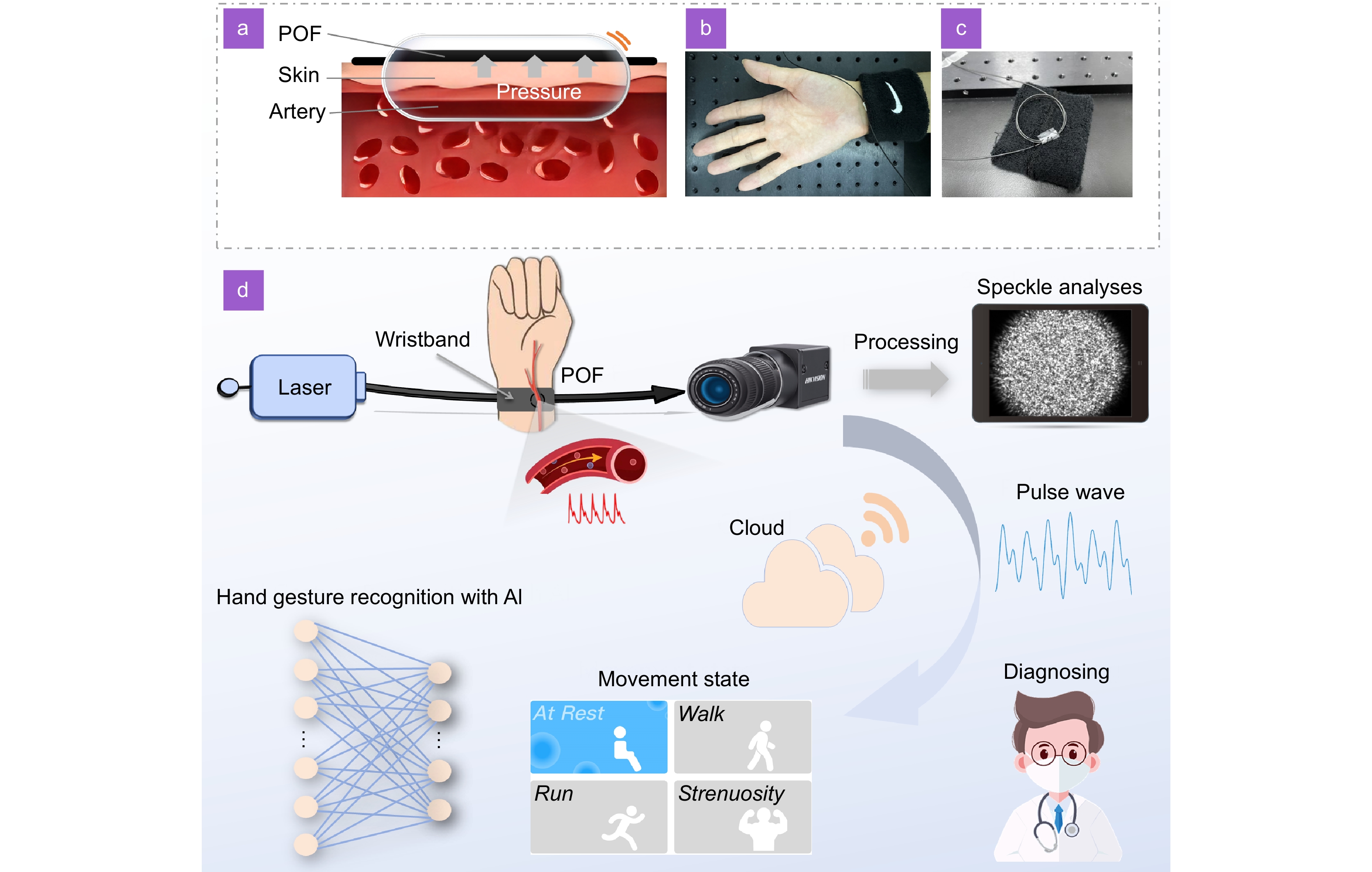
Figure 1.
Schematic diagram of the overall design. The diagram illustrates (a) the sensing principle of the smart photonic wristband. (b) The physical view of the wristband POF-based sensor. (c) The internal structure of the sensor. (d) The monitoring system, which includes a laser (light source), POF wristband sensor, signal acquisition, data processing, pulse rate computation, cloud terminal, and an artificial intelligence processor.
-
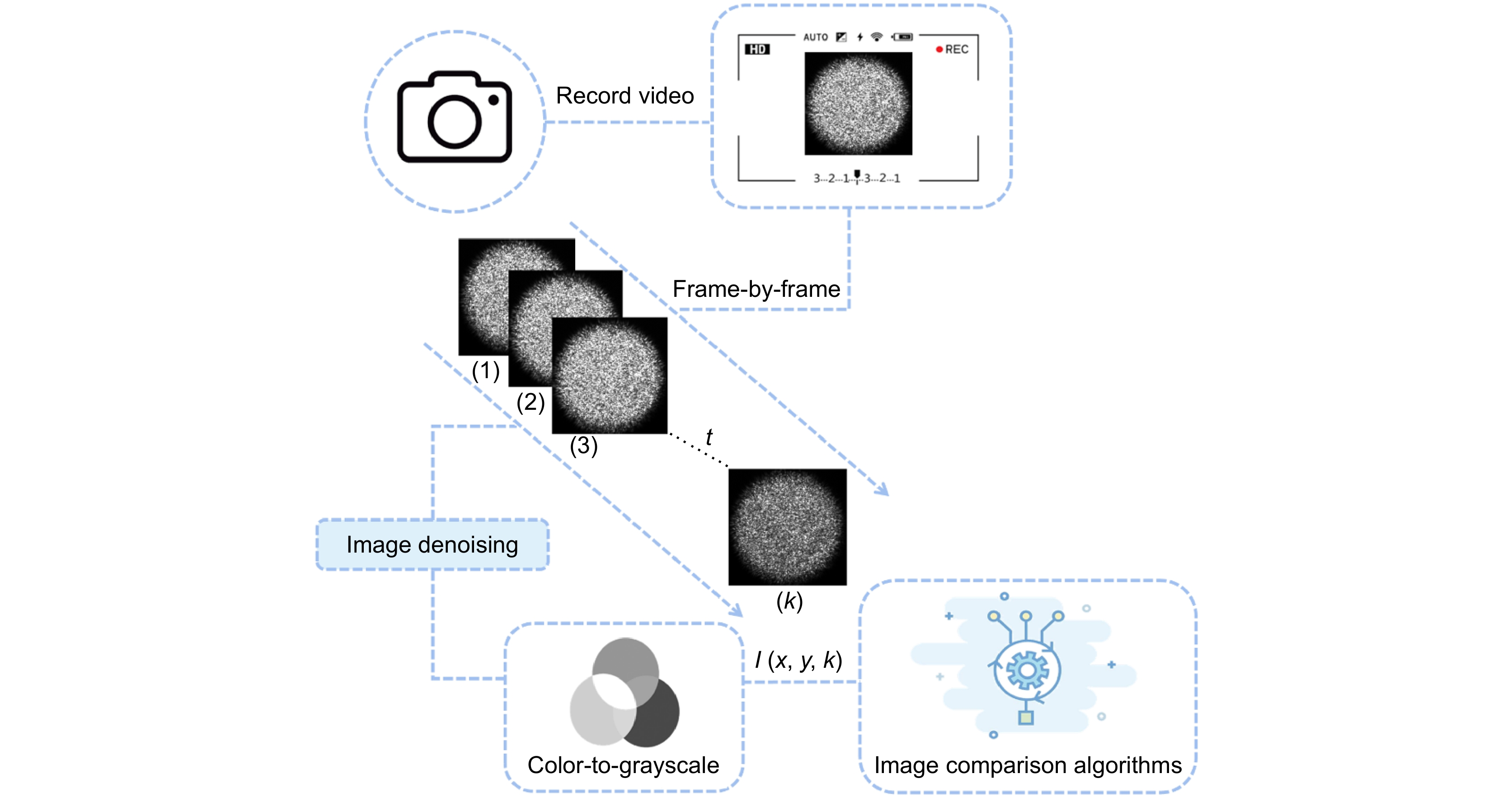
Figure 2.
Scheme of the specklegram image processing. The middle block diagram shows an example of the frame-to-frame difference under external continuous disturbances.
-
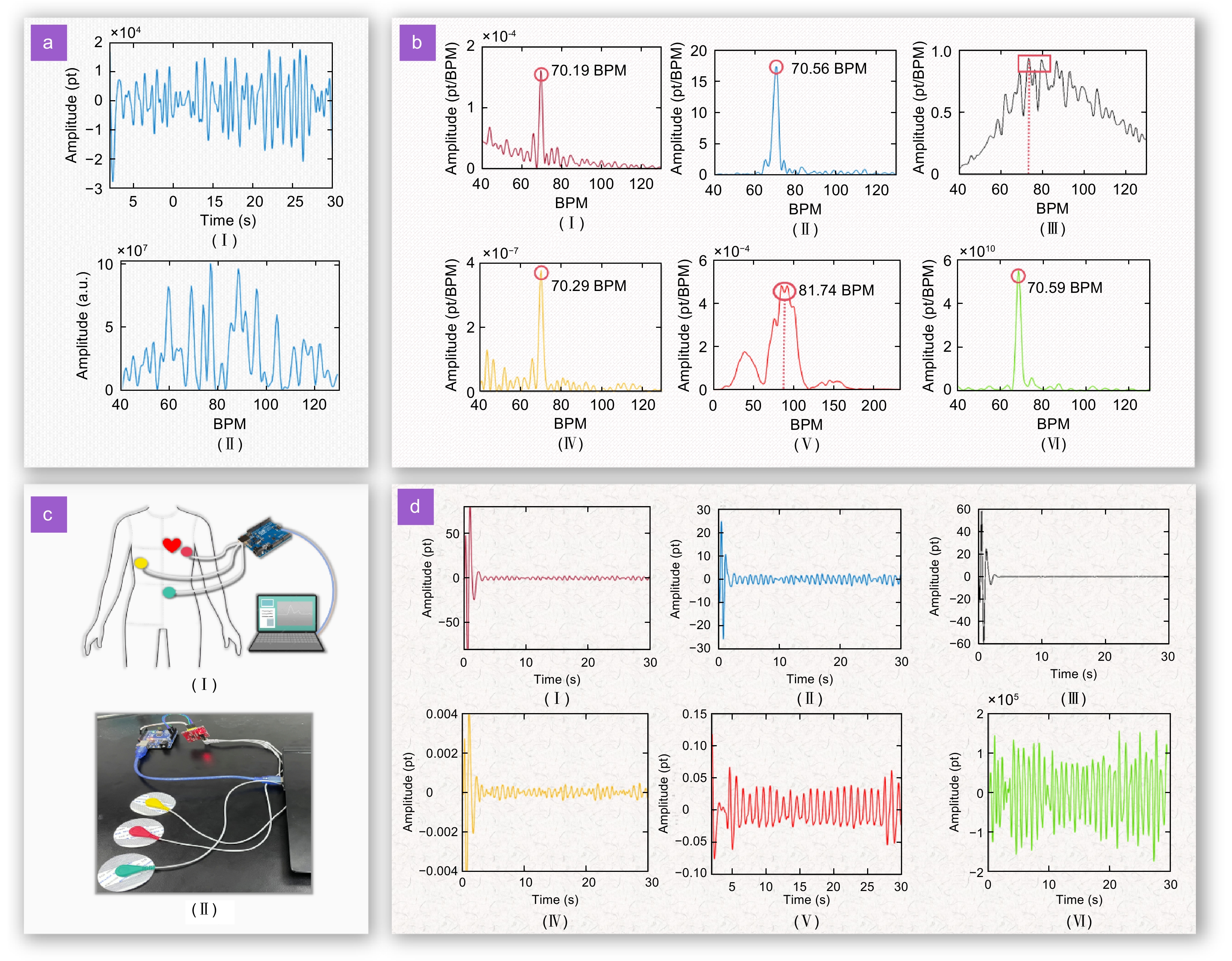
Figure 3.
Performance testing and optimization of the smart photonic wristband. (a) Results of a preliminary experiment: (I) Time-domain response of human pulse signal; (II) Power spectral density corresponding to the pulse signal. (b) Pulse waveforms from different processing methods. The method names corresponding to subscripts (I) to (VI) are normalized inner-product coefficient, zero-mean normalized cross-correlation, first-order moment, gray-level co-occurrence matrix, mutual information, and the sum of squared differences, respectively. (c) ECG reference signal acquisition device. (I) Schematic diagram; (II) Actual photograph. (d) Signal response in the frequency spectrum of different processing methods. The method names corresponding to subscripts (I) to (VI) are normalized inner-product coefficient, zero-mean normalized cross-correlation, first-order moment, gray-level co-occurrence matrix, mutual information, and the sum of squared differences, respectively.
-
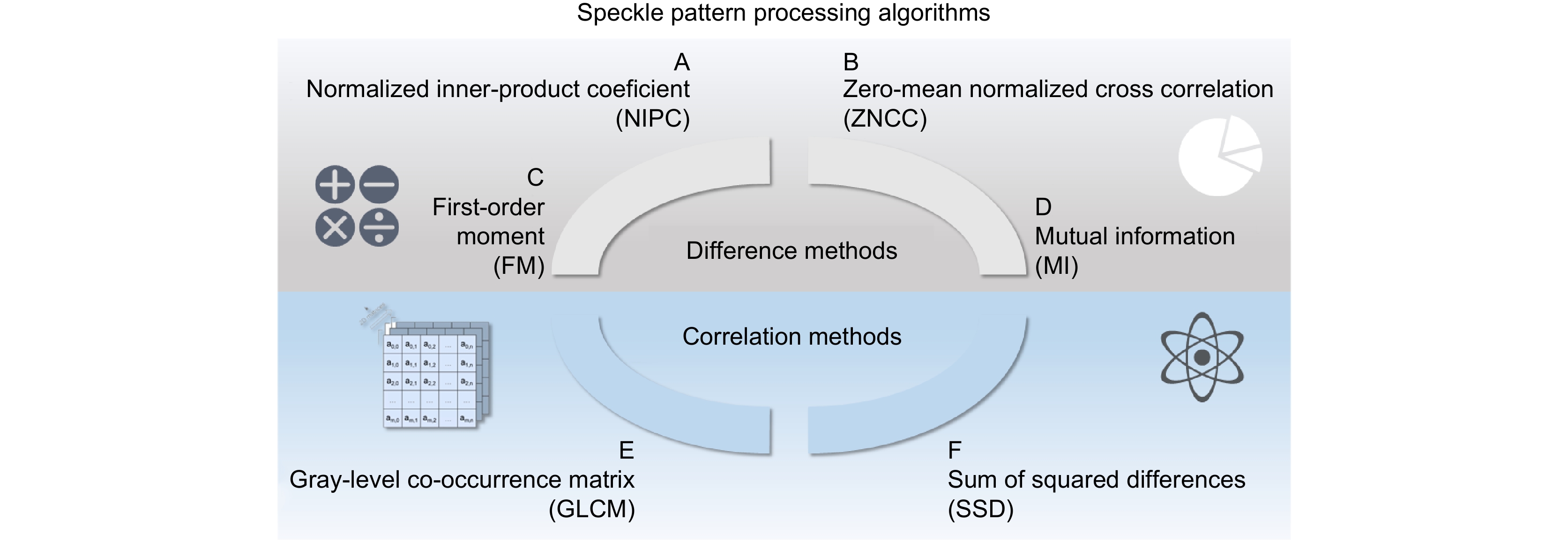
Figure 4.
Processing algorithms for speckle patterns using various methods.
-
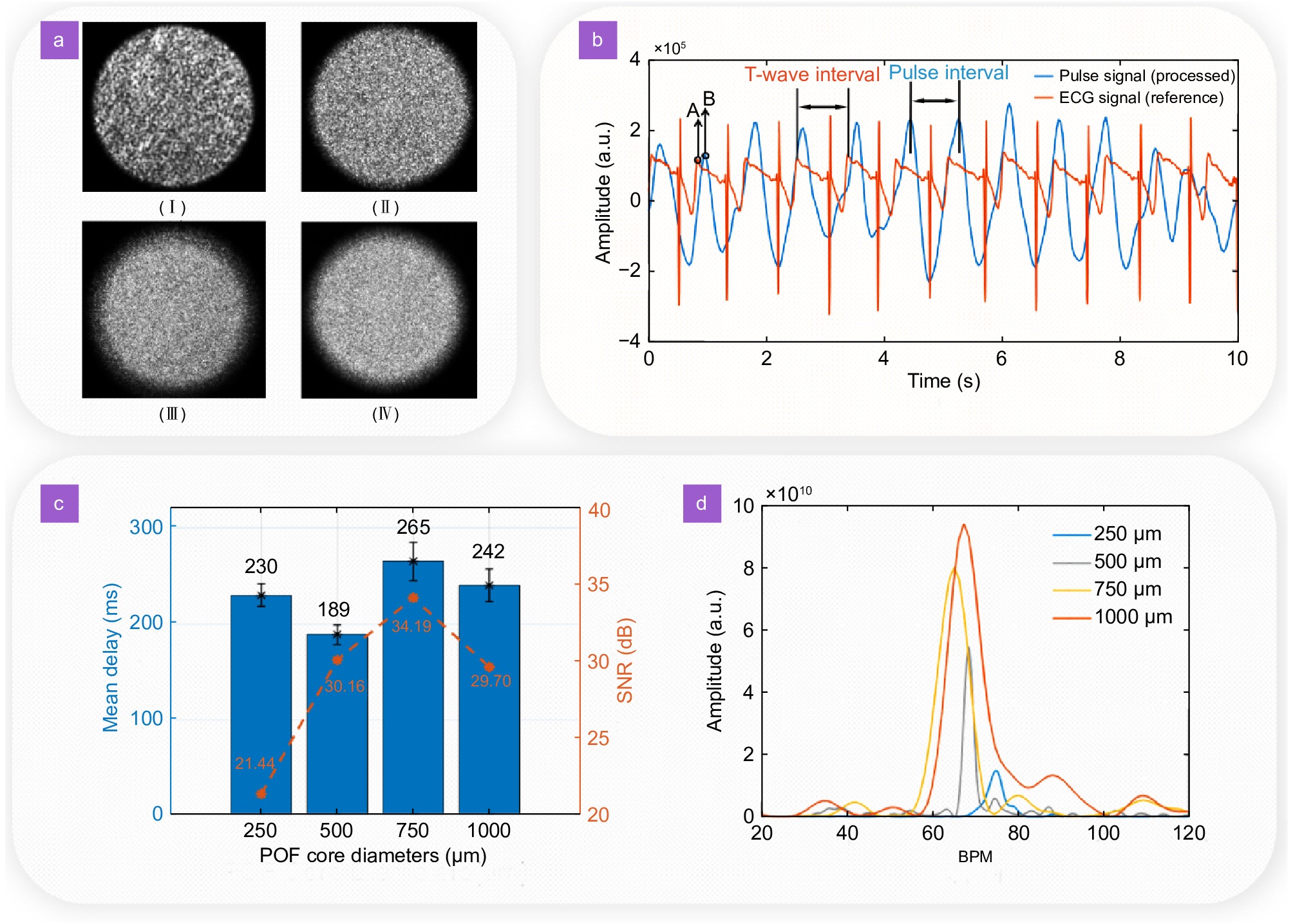
Figure 5.
(a) Speckle images formed by the POFs with different core diameters: (I) 250 µm; (II) 500 µm; (III) 750 µm; (VI)
1000 µm. (b) Example of a 10-s long comparison between a processed signal and a reference signal, where A is the T-wave peak in the ECG signal and B is the percussion-wave peak in the pulse signal. (c) Some results of the tested different core diameters, where the left ordinate is the time delay and the right ordinate is the SNR. (d) Signal response in the frequency domain with the different core diameters. -
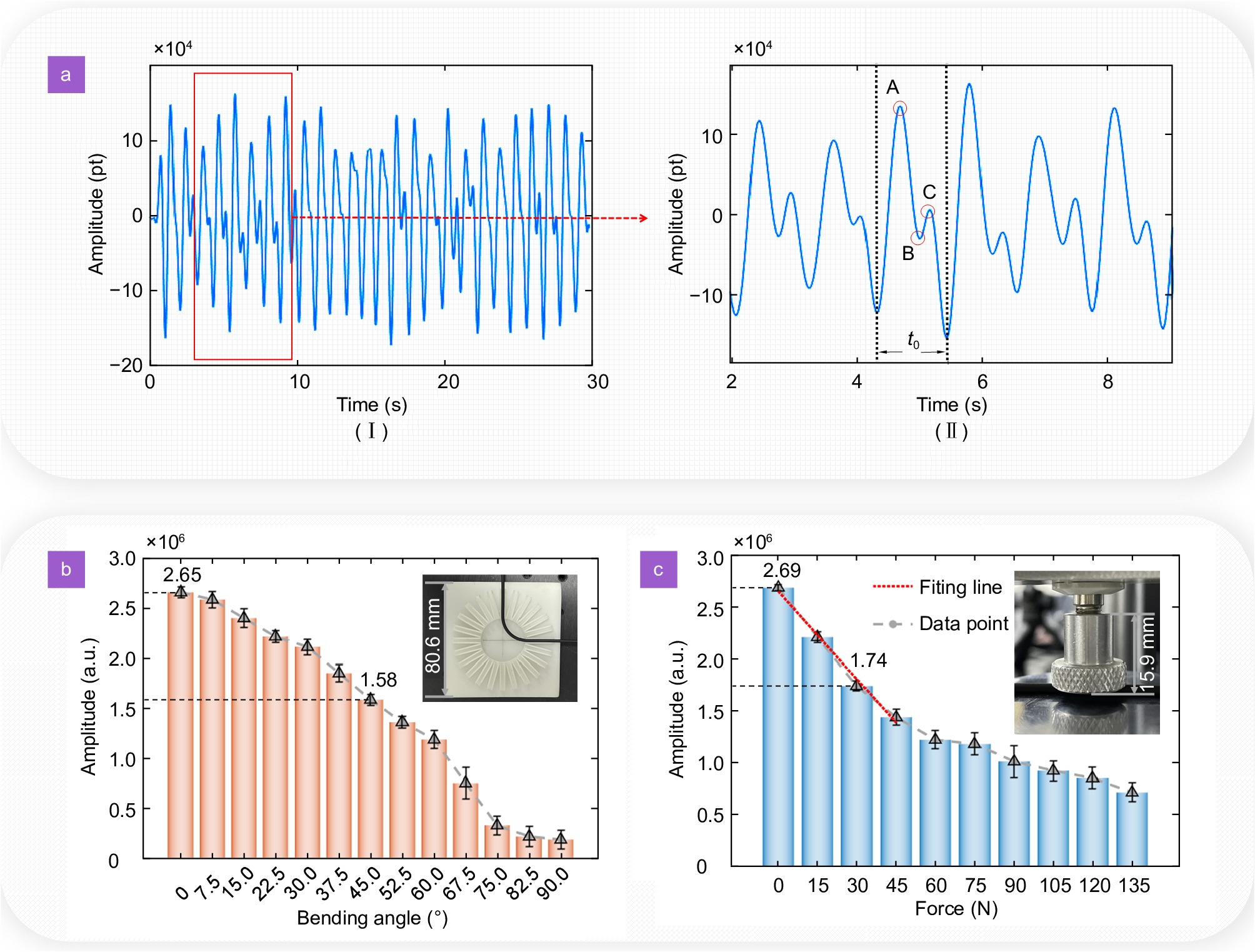
Figure 6.
(a) (I) Human pulse signal diagram acquired under the optimal method; (II) Detail within 10 s; A is the percussion wave (PW), B is the dicrotic notch, and C is the dicrotic wave. (b) Optical power-pressure curves of POF sensors in indentation tests. (c) Relationship between optical power and bending radius of POF sensor in bending tests.
-
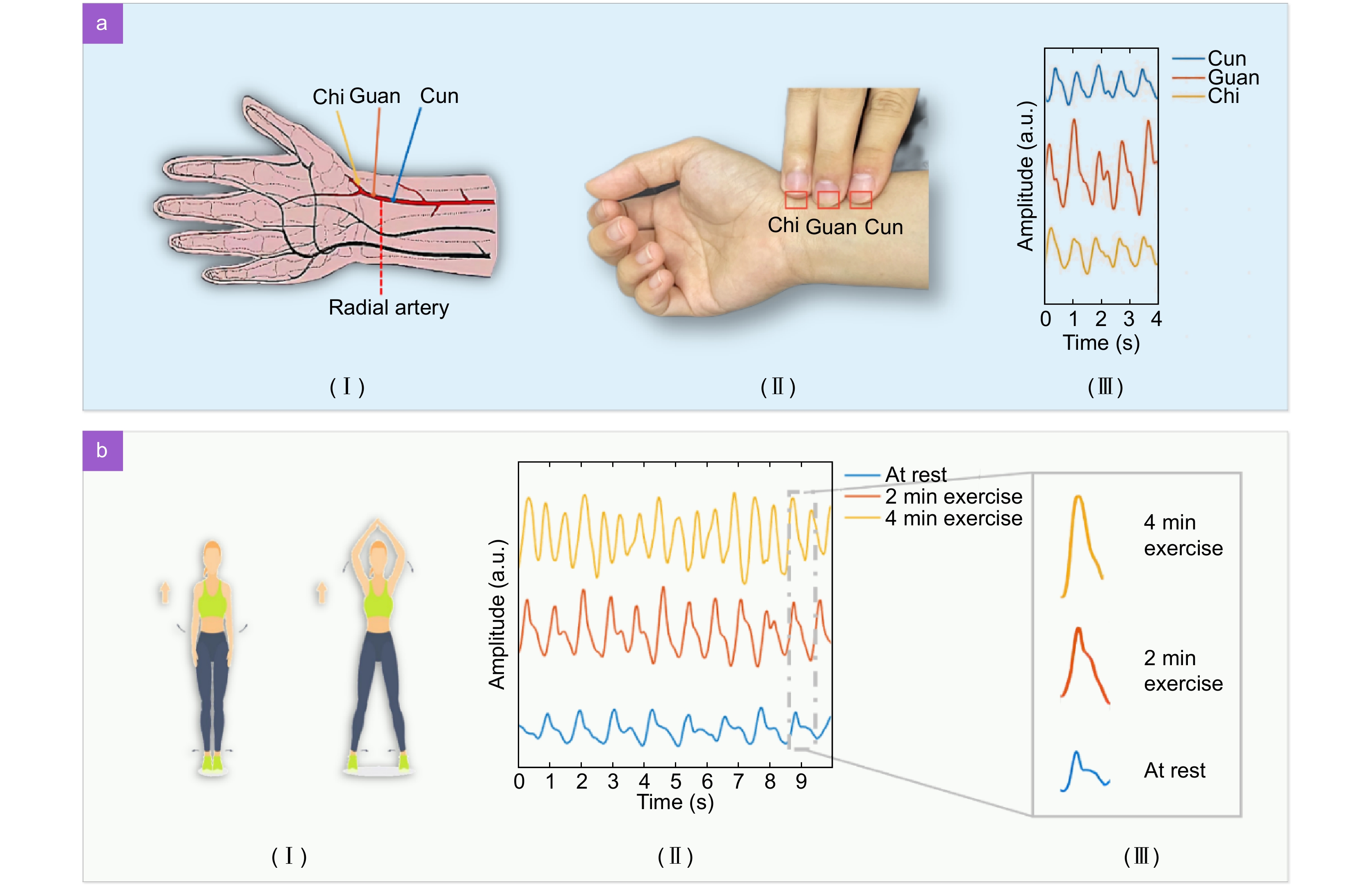
Figure 7.
(a) Diagnostic method of the Cunkou illustration. (I) Schematic illustrating the position of Cunkou. (II) Pulse waveforms at different positions of Cun, Guan, and Chi. (b) Pulse monitoring pre- and post-exercise. (I) Exercise example schematic. (II) Pulse waveforms at different exercise durations. (III) Waveform details in different states.
-
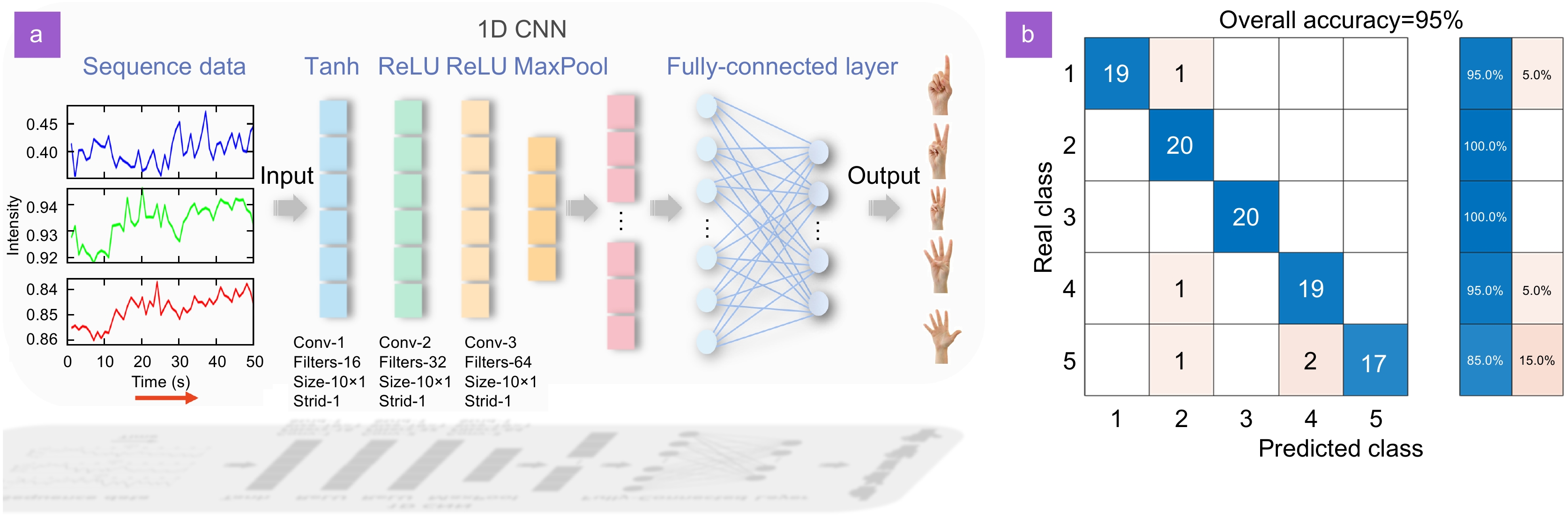
Figure 8.
Flowchart of the neural network model and classification results. (a) Neural network processing flow of the pulse wave signal. (b) Confusion matrix resulting from data processing.
-
Figure 9.
A snapshot of the smartphone application for monitored data visualization.

 E-mail Alert
E-mail Alert RSS
RSS


 DownLoad:
DownLoad: